In case you forgot about your annual PEPPER report, CMS has not. CMS has directed the PEPPER team to resume distribution of PEPPER reports to all post-acute facilities. The SNF Q4FY report will be delivered on July 29, 2020. It was originally scheduled for release on April 6, 2020 but it was held at that time due to the COVID-19 pandemic.
There’s also an updated PEPPER User’s Guide – Eighth Edition. I encourage you/your team to download this resource and use it when reviewing your PEPPER report.
You’ll note this new target area on page 7 of the Guide:

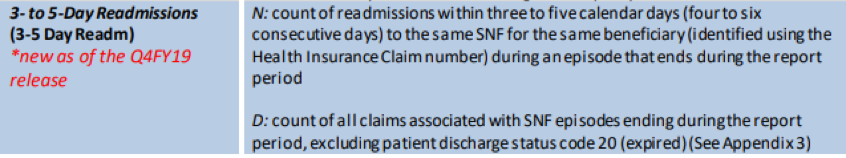
This new target area – 3-to 5-Day Readmissions – will provide data on the percent of readmissions just after the 3-day gap of non-coverage. The intent of this target area is to monitor the impact of the new CMS policy on interrupted stays related to discharge/readmission patterns.
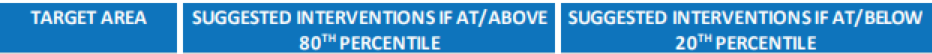
On page 10, you’ll find the corresponding interventions for this new item if your report reflects that you are at or above the 80th percentile:
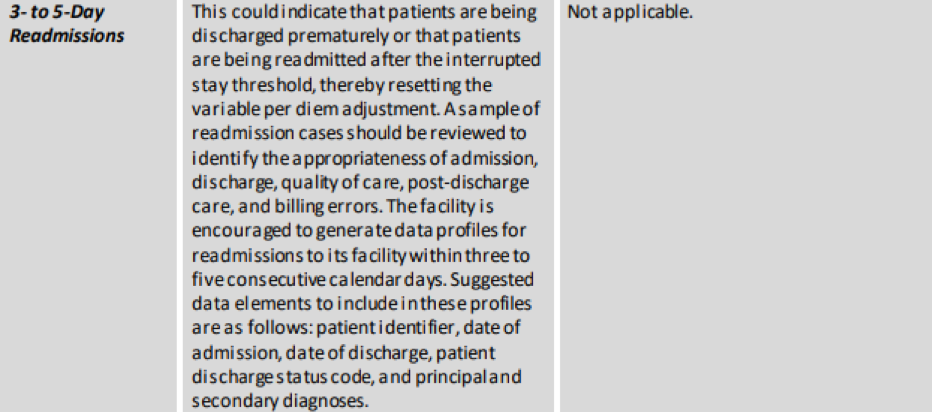
On page 21, you’ll find Appendix 3. This page provides examples of how readmissions are identified for inclusion in your PEPPER report:
These are additional resources for you to access:
- Training & Resources for Skilled Nursing Facilities
- Distribution Schedule – How to Get Your PEPPER
- SNF PEPPER Retrievals – PEPPER Resources Portal
- Accessing Your PEPPER through the PEPPER Resources Portal
Each SNF PEPPER summarizes claims data statistics (obtained from paid SNF Medicare UB-04 claims) for SNF episodes of care that end in the most recent three federal fiscal years (the federal fiscal year spans Oct. 1 through Sept. 30). In SNF PEPPER, a SNF is compared to other SNFs in three comparison groups: the nation, MAC jurisdiction and state. These comparisons enable a SNF to determine whether its individual results differ from other SNFs and whether it is at risk for improper Medicare payments (i.e., whether it is an outlier).
PEPPER does not identify the presence of improper payments, but it can be used as a guide for auditing and monitoring efforts. A SNF can use PEPPER to compare its claims data over time to identify areas of potential concern and to identify changes in billing practices. Your facility should be reviewing your PEPPER report every year – you can be certain that CMS is.




