Clients: You can access recordings of our client training webinars within your SimpleAnalyzer™ dashboard
Look for "Video Demos" in the "Help" section
What the latest Quality Measure updates mean for you
The removal of Section G from the new MDS version on Oct. 1, 2023, has impacted multiple Quality Measures used in the Five-Star Program or various state Quality Incentive programs. Simple has been hard at work implementing the new logic for these impacted QMs since the new specifications were published by CMS in late September. We are happy to announce that the new measures are now available in your Quality Measures reporting in the SimpleAnalyzer™.
Measures with a Seamless Transition
Six measures have very small modifications to the name of the items used. For example, N011 – Percent of Residents who Received an Antipsychotic Medication previously used N0410A as an indicator of antipsychotic medication received but uses N0415A1 to make the same determination on v18 assessments. These type of changes to the specifications are minimal enough that data collection and reporting will continue uninterrupted.
Other measures with similar changes include:
- N011 (SS) - Percent of Residents Who Newly Received an Antipsychotic Medication
- N029 (LS) - Percent of Residents Who Lose Too Much Weight
- N030 (LS) - Percent of Residents Who Have Depressive Symptoms
- N031 (LS) - Percent of Residents Who Received an Antipsychotic Medication
- N033 (LS) - Prevalence of Antianxiety/Hypnotic Use
- N036 (LS) - Percent of Residents Who Used Antianxiety or Hypnotic Medication
In SimpleAnalyzer you will not see any impacts to the collection or reporting of this data. The logic for these measures has been updated by Simple to look at the new v18 item numbers but the observed rates, numerator/denominator, 4Q averages, and Five Star scores will continue to be updated without disruption.
Measures with a Transition Quarter
There are two QMs which will undergo a much more significant modification. The removal of Section G from the comprehensive assessment has broken the data stream of the two long-stay measures tracking functional changes over the course of a resident stay.
In SimpleAnalyzer, these measures will also continue to calculate with changes to the logic being implemented behind the scenes. There are two significant differences with these measures compared to the first category though.
Transition Quarter
Because these measures require both a Target and Prior Assessment, 2023-Q4 will be a bit of a transition quarter where residents with v18 Target Assessment and v17 Prior Assessment will be excluded from the measure. This quarter will set the baseline level of functioning on these Section GG measures which will impact your performance when compared to the next comprehensive assessment.
Five-Star Score Freeze
The observed rates, numerator/denominator, and 4Q averages for these measures will continue to update in SimpleAnalyzer using the new logic but the Score for these measures (highlighted in blue below) will be held constant beginning in 2023-Q4 in line with CMS guidance. This Five-Star score freeze is to allow time to collect a full four quarters of data using the new measure logic.
Measures being Retired/Replaced
Three measures are so heavily impacted that they are being retired completely and replaced by new measures which operate according to a new measure definition.
- N045 – Percent of Residents with Pressure Ulcers is replacing the previous N015 – Percent of High-Risk Residents with Pressure Ulcers measure.
-
- The main difference between these two measures is the expansion of the measure to track pressure ulcers for all residents instead of only those considered high-risk. The new measure looks at the entire Long Stay resident population and risk adjusts based on seven covariates from the assessment.
-
- N046 – Percent of Residents with New or Worsened Bowel or Bladder Incontinence is replacing the previous N025 - The Percent of Low-Risk Residents Who Lose Control of Their Bowel or Bladder measure.
-
- This new measure looks at the entire Long Stay resident population to identify worsening bowel or bladder incontinence instead of looking more narrowly at only low-risk residents.
-
- S042 – Discharge Function Score is replacing the previous N037 – Residents Who Made Improvements in Function measure.
-
- This new measure is a major departure from the previous short stay measure. This QRP type measure compares ten items from Section GG on a SNF PPS Discharge to evaluate whether the resident reached the CMS defined expected discharge goal set by the matched PPS 5-Day assessment.
-
Five-Star Removal Impact
In SimpleAnalyzer, the old measures (N015, N025, and N037) will continue to be included in the list of measures. The Five-Star impacting data points will continue to be held constant until further information from CMS on how the new measures will be used to impact the provider Five-Star rating.
Five-Star Addition Impact
You will also see the new measures (N045, N046, and S042) on new QM cards within SimpleAnalyzer. These measures will begin data collection starting with 2023-Q4 so providers can track performance even before they impact Five-Star calculations. Be sure to familiarize yourself with N045 and S042 over the next few quarters before they are included in the Five-Star program.
Five-Star Freeze Timeline
Now that we understand the impact of the v17 to v18 transition to each metric individually, it is important to understand how our overall Five-Star rating will be impacted. The graphic below is a visual summary of the revised CMS memo from October 2024 which summarizes the changes to accommodate these changes.
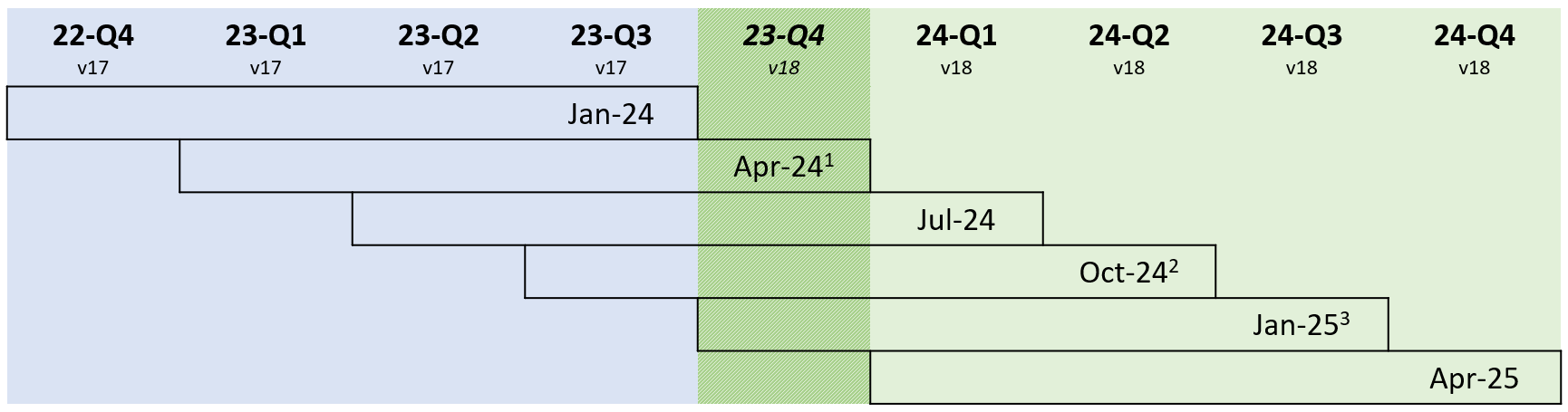
- The April 2024 refresh (with data from 2023-Q1 to 2023-Q4) is the first month to include data which has a mix of v17 (blue) and v18 (green) assessment types. This is the first quarterly refresh which will be impacted and, as a result, the four QMs used to calculate the Five-Star score for each of the impacted metrics will be held constant.
- CMS originally targeted the October 2024 refresh to start publishing the rates and points derived from the new S042 Expected Discharge Score but has since announced that the measure will be published along with the others in January 2025 instead.
- CMS intends to publish data from all four impacted measures in January 2025.
One important note about this plan. The January 2025 publishing date would include data from 2023-Q4 which is heavily impacted by the transition quarter discussed above. Keep an eye out for communication from CMS that might revise this timeline to target April 2025 as the first refresh with updated rates and scores to avoid the impact of the 2023-Q4 transition quarter.
Conclusion
There are a lot of moving parts for providers with these enormous MDS version changes. Simple is committed to quickly and accurately interpreting these changes in our application and we appreciate your partnership as we all get our bearings in this new environment. Please don’t hesitate to reach out with questions or concerns as you explore these changes in our application.








4 Comments on “[IMPORTANT] Quality Measure updates in SimpleAnalyzer™”
When will the recording of this Webinar be available
Hi Deb — The recording is now available within SimpleAnalyzer on the Help tab. Thanks!
Hello,
I pulled my information after watching this webinar and reading through the article and I have a patient that is triggering for the new S042 QRP that was a discharge home with hospice. The End of PPS assessment has A2105=09 which according to the QRP manual should be an exclusion. Is this a SimpleLTC error or am I missing something else? Thanks for your help
Hi Jamie: Please reach out to our Support Team so they can help you with this specific question. You can contact them via phone or the NetsmartCONNECT portal (see info under “Get support” on this page). Thanks!