- Updated county positivity rates are now available: Week Ending September 17, 2020. Archived county positivity data is found here.
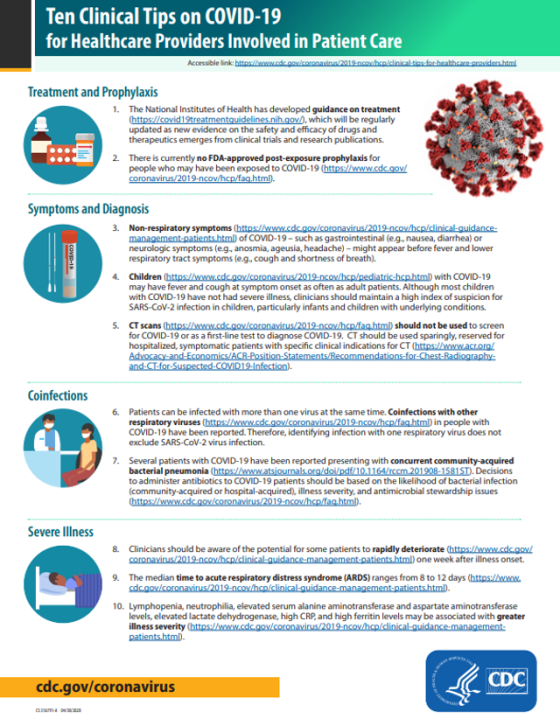
- Ten Clinical Tips on COVID-19 for Healthcare Providers Involved in Patient Care for Healthcare Workers was updated by CDC on September 16, 2020. Areas covered include: Treatment and Prophylaxis, Symptoms and Diagnosis, Co-Infections and Severe Illness. There’s also a downloadable Fact Sheet that provides a great visual to these tips.
- An interesting study - Association Between CMS Quality Ratings and COVID-19 Outbreaks in Nursing Homes conducted in West Virginia NHs from mid-March to mid-June of 2020 showed that “Compared with 1-star–rated (lowest rating) nursing homes, the odds of a COVID-19 outbreak were 87% lower among 2- to 3-star–rated facilities and 94% lower among 4- to 5-star–rated facilities. CMS star ratings can serve as proxy indicators for COVID-19 outbreak risk; health departments could use them to identify priority nursing homes and inform the allocation of infection prevention and control resources.”
- I proffer another interesting study and subsequent paper, which casts doubt on the above study. Relationship between nursing home COVID-19 outbreaks and staff neighborhood characteristics. “These results suggest that staff communities are likely to be an important source of infection, and that disparities in nursing home outbreaks may be related to differences in the types of neighborhoods nursing home staff live in.” This is a 17-page interesting read authored by Karen Shen (PhD candidate, B.S., M.S.), Department of Economics, Harvard University, Cambridge, MA. This study used an eighteen-state sample of nursing homes to study facility-level determinants of COVID-19 outbreaks, measured as the number of deaths per bed. The focus is on within-county differences in outbreak sizes. The above study was conducted within the state of West Virginia. This study was done in July while the WV study was mid-March to Mid-June.
Conclusion: “Which nursing homes experienced the largest outbreaks of COVID-19 within a county was not random, but it was also not largely determined by other measures of quality commonly cited in the nursing home literature, such as star rating. Instead, a key determinant was the characteristics of the neighborhoods where nursing home staff members lived—facilities whose staff lived in denser, less white neighborhoods with more public transportation use have had significantly more deaths than other facilities in the same county.”
This study provides credence for facilities looking beyond the positivity of the county where the nursing home physically resides. The positivity of the counties their staff reside in should also determine the frequency of COVID-19 testing for staff. Page 5 of QSO-20-38-NH speaks to this:
“The guidance above represents the minimum testing expected. Facilities may consider other factors, such as the positivity rate in an adjacent (i.e., neighboring) county to test at a frequency that is higher than required. For example, if a facility in a county with a low positivity rate has many staff that live in a county with a medium positivity rate, the facility should consider testing based on the higher positivity rate (in scenario described, weekly staff testing would be indicated).”
Want to keep up with the changing COVID-19 situation in skilled nursing?